Postpartum running is like training for a marathon, the more time you put into it, the more successful you will be. To allow for healing to occur to your body post-baby, wait at least 12 weeks postpartum until you begin running. In the meantime build a strong strengthening foundation so you can avoid injury. Now let’s dive into a common question, I get asked by women I work with: “Should I run with diastasis recti?”
What is Diastasis Recti (DR)?
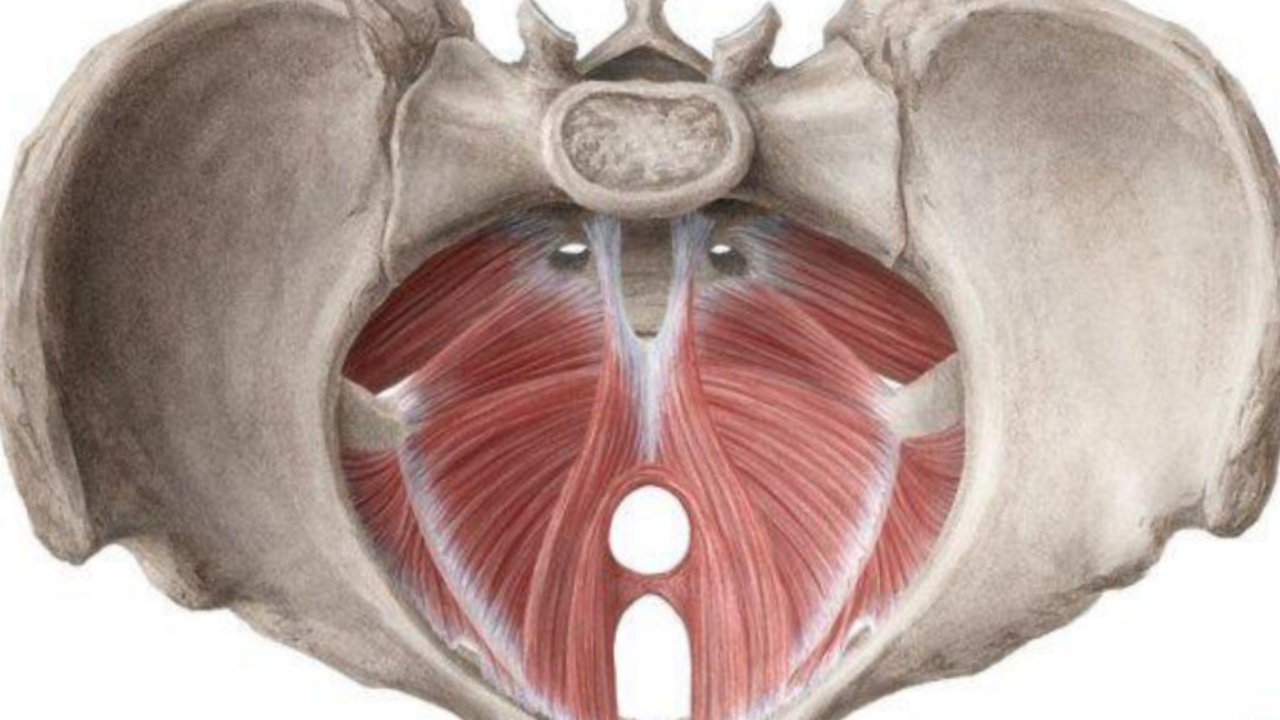
Diastasis recti abdominis (DR) is the thinning of the linea alba and separation of the two muscle bellies of the rectus abdominis muscle, or the “six-pack ab” muscle. It happens to 100% of women during their pregnancy but can vary at different degrees of separation.
The research on why it is more severe in some women compared to others is scarce, but some factors can include higher maternal age, high birth weight, multiple pregnancies, ethnicity, and weight gain, to name a few. DR can dramatically impact the stability and integrity of your core muscles and can cause multiple other problems including low back pain or pelvic floor dysfunction if the DR does not heal. The good news is, you can get better with physical therapy and a good exercise plan.
How do I know if I have DR?
You may notice doming or coning along the midline of your abdominals, especially when performing certain exercises or when you go to sit up in bed. You can also check it yourself by following the steps in the video below.
Diastasis that seems deep or wide does have the potential to heal and you can avoid surgery by doing core and full-body strengthening exercises under the guidance of a physical therapist. If it does not seem very wide and there is mild tension in your abdominals, most of the time it can heal naturally and regains tension after pregnancy and it closes on its own.
Doing core exercises and reconnecting to this area, can be very beneficial postpartum (PP), making carrying and lifting your growing baby easier.
You are not alone! 60% of women have a DR by 6 weeks PP with the primary location at the umbilicus. It is recommended to have your DR assessed by a physical therapist if you have a concern. If you are a very active individual, it is advised to have it assessed in both a lying down position and in standing in a loaded position (plank against a wall). This will help determine how your core responds when more work is required.
DR is not just a core problem
DR can affect your entire body, including your posture, your strength, and your breathing pattern. Therefore, starting with 360 breathing exercises, progressing to core strengthening, and working on your posture while standing and running is important.
Alignment of your feet, knees, pelvis, ribs, and head and neck can all affect DR and that is why seeing a physical therapist to address any concern you may have is key! A lot of what we do daily requires our core to work and function appropriately and with a DR our core is somewhat compromised. The first thing you can try to work on is an even breathing pattern and to maintain an even breathing pattern while performing more strenuous household chores. You can start this in your early weeks PP.
What can I do to heal my DR:
Things you can work on before you start running are:
1) 360 breathing
Are you able to get air into your entire rib cage, front, sides, and back while lying down and in standing?
2) Be more mindful of your posture throughout the day.
Are you standing equally on both legs? Are you able to keep your ribs over your pelvis or pelvis under your ribs? Stay tall and keep good alignment
3) Strength training
Consider adding a full-body strength training routine into your week, be sure you can breathe through each exercise and that you are progressing mindfully for your body
4) Balance
Are you able to stand on one leg for at least 30 seconds? Are you able to perform exercises that require you to stand on one leg without losing your balance? Can you maintain an even breathing pattern while performing them or do you hold your breath?
How to return to running safely with a DR
If you have been diagnosed with DR, it is something you can start working on immediately PP. As you approach your 12th week postpartum, you can begin returning to running through a progressive run-walk program. In conjunction, working on some of the above suggestions would be very helpful in your recovery. Long story short, some women may run safely with a diastasis if they have taken the steps to heal it and are still working on strengthening. BUT, if you have any symptoms of leaking, pressure, pain, or heaviness in the pelvic floor, then please stop and consult a physical therapist or your OBGYN.
So when you ask the question, should I run with diastasis recti, the answer is you can run and be stronger than ever, but be sure to take the time to recover from your pregnancy and develop a strengthening routine.
My goal in writing about diastasis and running is that you do not have to be afraid to run again if you have diastasis. Follow these steps and you will be back to running in no time!
You are strong and you are capable,
Dr. Juliana
P.S Are you ready to run? Let’s chat- book a free discovery call with me.
Resources:
- Diastasis Recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors, and report of lumbopelvic pain. Sperstad, J et al. Department of Sports Medicine, Norwegian School of Sports Sciences. 20 June 2016.
- Mota, P., Pascoal, A.G., Carita, A.I., & Bø, K. (2015). Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Manual Therapy, 20(1), 200-205.